The diagnosis of pancreatitis often leaves patients with more questions than answers. It’s a complex condition shrouded in medical jargon and uncertainty. In this unique conversation, Harsh Gupta, a former patient who found lasting relief at Padaav, sits down with Vaidya Shikha Prakash to ask the common questions that arise from his own experience and from the public. This is a journey to empower you with the right knowledge.
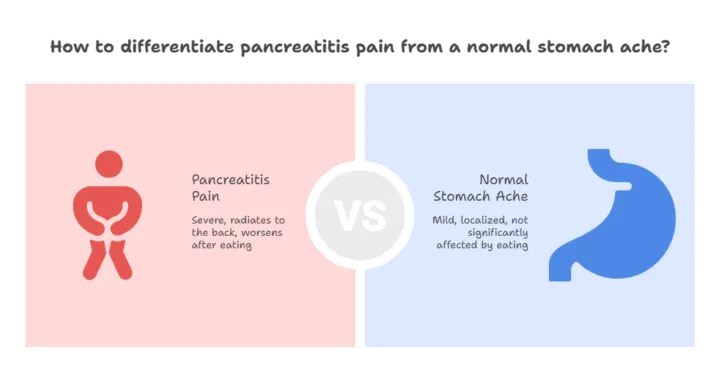
The Pain: Pancreatitis vs. a Normal Stomach Ache
The pain of pancreatitis is often mistaken for a common stomach ache, but it’s fundamentally different. While a regular stomach ache might be mild or uncomfortable, pancreatitis pain is typically acute and agonizing. Vaidya Shikha Prakash outlines the distinguishing factors:
- Intensity: The pain is severe and not to be taken lightly.
- Location: It usually starts on the left side of the abdomen and radiates to the back.
- Triggers: The pain worsens significantly after eating.
So, how do doctors confirm a pancreatitis diagnosis? It begins in the emergency room for severe pain. The most important initial blood tests check for elevated levels of amylase and lipase, with lipase being a particularly sensitive indicator. An ultrasound is often done first, and if inflammation is visible, further imaging like a CT scan or MRI/MRCP may be ordered to assess the severity and potential complications like necrosis. These advanced scans are especially crucial because the pancreas is a retroperitoneal organ, often hard to visualize clearly with a standard ultrasound.
What is the link between high triglycerides and pancreatitis? Triglycerides are fat molecules that circulate in the blood, storing excess calories. Vaidya Shikha Prakash confirms that a very high level can lead to pancreatitis. While a level below 150 mg/dL is considered ideal, a level above 500 mg/dL can trigger an attack, and a level over 1000 mg/dL almost certainly will. She has observed this pattern not just in middle-aged individuals but also in some very young children.
Can viral infections like COVID-19 trigger an attack? Harsh’s personal experience with COVID-19 led him to question if it was the cause of his severe attacks. Vaidya Prakash explains that any viral infection places stress on the body, which can trigger a pancreatitis flare-up. She notes that medical research has shown an increase in pancreatitis cases following COVID-19 infections.
Can pancreatitis lead to diabetes? Yes, it can. The pancreas has a dual function: it produces both digestive enzymes and insulin. The inflammation and damage from pancreatitis can harm the insulin-producing cells, leading to a specific type of diabetes known as Type 3c or pancreatogenic diabetes. This can be a temporary complication that resolves as the inflammation subsides, or in some cases, it can become a permanent condition.
Long-Term Management: Navigating Fear and Recovery
What about procedures like ERCP? ERCP is a procedure used for both diagnostic and curative purposes, for example, to clear blockages or place stents. However, because the pancreas is a very sensitive organ, Vaidya Prakash warns that ERCP can, in a small percentage of cases, cause a post-procedural complication that leads to a severe acute pancreatitis attack, including necrosis.
Do I need regular tests after recovery? Harsh’s fear of a relapse led him to ask if he should get routine blood tests or scans. Vaidya Prakash advises against this unless a symptom is present. She explains that if you feel fine, your reports will likely be normal anyway, and constantly checking them is often a psychological need. The only time a CT or MRI might be needed after recovery is if there is an underlying progressive condition that requires long-term monitoring, and this should only be done under a doctor’s guidance.
When should I go to the hospital? The final, crucial question is when to seek immediate medical help. The answer is straightforward: you should definitely go to the doctor if you experience severe, unmanageable pain and are not under a doctor’s supervision or in a structured treatment program.
Harsh concludes by emphasizing the importance of having the right information. Pancreatitis is not a disease to be feared if you are well-informed and take the right steps. It is a manageable condition, and with the right care, you can live a healthy life.
The journey with pancreatitis is one of knowledge over fear. By understanding your body and seeking expert guidance, you can regain control and live a life free from constant worry.