Pancreatitis can be a terrifying diagnosis, but understanding the disease is the first step toward recovery. Whether you have had one attack or suffer from recurrent episodes, your lifestyle and choices play a massive role in your healing journey.
Here is a simple guide to the most common questions about managing Pancreatitis.
1. What is the very first step to prevent a second attack?
If you have had one attack, the most critical step is identifying your specific Risk Factors. Pancreatitis isn’t the same for everyone. You must work with your doctor to find out what triggered yours:
-
Is it gallstones or gallbladder sludge?
-
Is it alcohol consumption?
-
Is it high triglycerides (fat in the blood)?
-
Is it a side effect of a medication?
Once identified, the goal is to remove that trigger entirely from your life. If no cause is found, it is called Idiopathic Pancreatitis, which requires a deep dive into your daily routine, eating habits, and stress levels.
2. Why is Hydration so critical?
Dehydration is a major, often overlooked trigger for Pancreatitis attacks. Here is why:
-
Enzyme Concentration: When you are dehydrated, your pancreatic juices become thick and viscous. This makes it harder for enzymes to flow, leading to inflammation.
-
Toxin Removal: Water is essential for flushing toxins out of your body. Without enough water, these toxins build up and stress the pancreas.
-
The Standard: You should aim for 2 to 2.5 liters of water daily. This helps maintain the right consistency of digestive enzymes and prevents the “viscosity” that triggers attacks.
3. The Diet: What must go and why?
To protect your pancreas, you must remove foods that put “systemic stress” on the organ. Avoid:
-
Excessive Oil & Fried Foods: The pancreas has to work overtime to produce enzymes to break down heavy fats.
-
Heavy Spices & Processed Sugar: These cause inflammation and are difficult for a sensitive system to process.
-
Irregular Eating: When you eat is as important as what you eat. Skipping meals or eating late at night puts immense pressure on your digestive system.
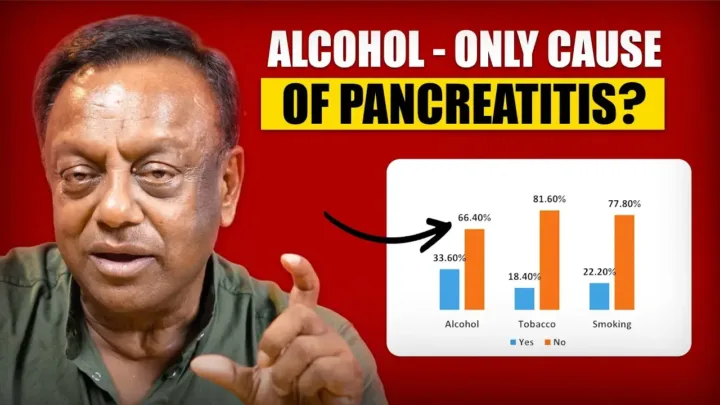
4. Understanding Common Triggers
-
Gallstones: Small stones or “sludge” can block the pancreatic duct. This causes digestive enzymes to flow backward into the pancreas, leading to “Auto-Digestion”—where the pancreas literally starts digesting itself.
-
Alcohol: It thickens pancreatic juices and causes systemic dehydration, leading to immediate inflammation.
-
Smoking: Nicotine restricts “micro-circulation” in the pancreas and creates oxidative stress, which directly triggers inflammation.
-
Obesity: Excessive weight leads to high cholesterol and triglycerides, which are primary fuel for pancreatic attacks.
5. Why do patients need Insulin or Digestive Enzymes?
In Chronic Pancreatitis, the organ may begin to fail in two ways:
-
Exocrine Failure: The pancreas can’t make enough enzymes to digest food. Symptoms include bloating, foul-smelling stools, and dull pain. In this case, Digestive Enzymes are prescribed.
-
Endocrine Failure: The pancreas stops producing enough insulin, leading to Type 3c Diabetes. This usually requires Insulin therapy to manage blood sugar.
6. The Problem of Malnutrition
Many Pancreatitis patients suffer from vitamin deficiencies (A, D, E, and K). Because these vitamins are fat-soluble, and patients are often on a low-fat diet, the body struggles to absorb them. This can lead to poor vision, weak bones (osteoporosis), and low immunity. Supplementation under medical guidance is often necessary.
The Padaav Perspective: When there is no clear cause
At Padaav, we see many “Idiopathic” cases—patients who don’t drink, have no stones, and no genetic history. In these cases, the “root cause” is often a disturbed lifestyle:
-
Poor sleeping patterns (night routine).
-
Untimely eating.
-
High-stress behavior.
The Bottom Line: Pancreatitis management is a partnership between the doctor, the medicine, and the patient. By correcting your hydration, diet, and daily routine, you can stop the cycle of attacks and regain your health.