Pancreatitis is a complex disease that often remains unknown to patients until they or a loved one receives a diagnosis. Unfortunately, confusion and misinformation surround the condition, making effective management difficult.
Vaidya Shikha Prakash addresses the most common myths, clarifying the reality of Pancreatitis based on clinical experience and Ayurvedic wisdom.
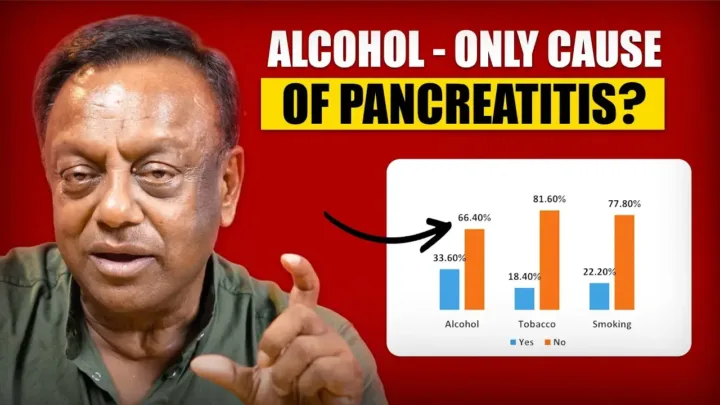
The Alcohol Stigma and Root Causes
Myth 1: Pancreatitis is caused ONLY by alcohol.
The Reality: This is a huge myth. While alcohol is a known trigger, it is not the only cause. Pancreatitis can be idiopathic (unknown cause), genetic, autoimmune, drug-induced, or caused by obstructions and toxic exposure.
Myth 2: Beer or wine are safer than hard liquor for the pancreas.
The Reality: No. This is a dangerous misconception. No form of alcohol whether beer, wine, or hard liquor is safe for a patient with Pancreatitis. Alcohol and the pancreas have a direct negative connection, and consumption must be completely abandoned.
Myth 3: High Triglycerides are just a lab report, not a real cause.
The Reality: High triglycerides are considered a major cause of Pancreatitis. They are a sign that fat metabolism is distorted, a process in which the pancreas plays a key role. It’s not the sole cause, but a significant risk factor, alongside genetics, obesity, and poor diet.
Addressing Triggers and Misdiagnosis
Myth 4: Acute Pancreatitis is impossible without gallstones.
The Reality: Gallstones or sludge in the gallbladder are a major cause, often requiring surgery. However, gallstones are not the only cause. Many patients experience recurrent attacks even after gallbladder removal, confirming that other factors are at play.
Myth 5: Medications never damage the pancreas.
The Reality: This is false. Many common medications can trigger Pancreatitis. Vaidya Shikha Prakash notes that this can include:
-
Excessive use of certain antibiotics.
-
Some steroids (even when taken in controlled doses).
-
Certain fat-loss medications.
Myth 6: Spicy food is the direct cause of pancreatic damage.
The Reality: Spicy food alone is not the direct cause. However, highly spicy, heavy, or rich food can lead to acidity, bloating, and heaviness, which can trigger pain and worsen the disease. Patients are always advised to prioritize simple, nourishing food over intense flavor.
Demographic and Progressive Facts
Myth 7: Pancreatitis only affects older men.
The Reality: This is a huge myth. Pancreatitis affects both men and women equally. However, diagnosis can be delayed in women who often dismiss symptoms (like recurrent abdominal pain and vomiting) as minor issues, relying on painkillers.
Myth 8: Young people are safe from Pancreatitis.
The Reality: This is the biggest myth. Pancreatitis is highly prevalent in youth and is often considered a disease of the younger age group. Vaidya Prakash has seen the major age bracket shift from 18-45 to 10 to 35 years old, confirming it is very common in adolescents and young adults.
Myth 9: Smoking has no connection to the pancreas.
The Reality: Smoking has a direct connection to Pancreatitis. Anyone diagnosed with the condition should absolutely quit smoking immediately, regardless of the severity of the initial attack.
The Path to Recovery and The Padaav Approach
Myth 10: Chronic Pancreatitis patients cannot recover.
The Reality: Recovery is absolutely possible, especially for alcoholic patients, if they strictly adhere to comprehensive treatment. Simply quitting alcohol is NOT enough. Recovery requires addressing lifestyle, diet, and all other underlying causes. The patient’s sincerity is key to the success of the treatment.
Myth 11: Diabetes and Pancreatitis are unconnected.
The Reality: This is a major myth. The pancreas is the organ that secretes insulin. Pancreatitis can lead to Type 3c Diabetes, which is often uncontrolled or results in an early onset of diabetes requiring treatment. The two conditions have a direct, crucial connection.
The Padaav Solution:
Pancreatitis is a debilitating disease linked to suicidal tendencies due to its unpredictable nature and the myth that it is non-curable.
However, the disease can be successfully treated. By focusing on lifestyle, diet, and addressing the root causes (like genetics, infections, trauma, and drug-induced triggers), the condition can be stabilized and reversed. The solution is found in a commitment from the patient, doctor, and treatment working together to restore health.