Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) is a debilitating, long-term neurological disease that impacts millions worldwide. Far beyond ordinary tiredness, ME/CFS is a complex, multi-system illness that profoundly disrupts energy production and normal bodily functions, leaving individuals with severe and persistent symptoms. Despite its significant impact, ME/CFS remains largely underdiagnosed, with estimates suggesting that up to 90% of affected individuals may not have a formal diagnosis. This diagnostic gap represents a critical health crisis, leaving many suffering without proper medical validation, understanding, or support.
What is ME/CFS? A Biological Reality
ME/CFS is recognized as a real, biological disease, not a psychological condition. It is characterized by a substantial reduction in a person’s ability to do activities that were possible before the illness. This isn’t simply “feeling tired”; it is a pervasive, often overwhelming exhaustion that is not relieved by rest and significantly interferes with daily life.
The term “Myalgic Encephalomyelitis” itself points to potential underlying biological issues: “myalgic” referring to muscle pain and “encephalomyelitis” suggesting inflammation of the brain and spinal cord. While definitive neuroinflammation is an area of ongoing research, the name reflects the neurological and muscular symptoms commonly experienced by patients.
The Hallmark Symptoms: Beyond Fatigue
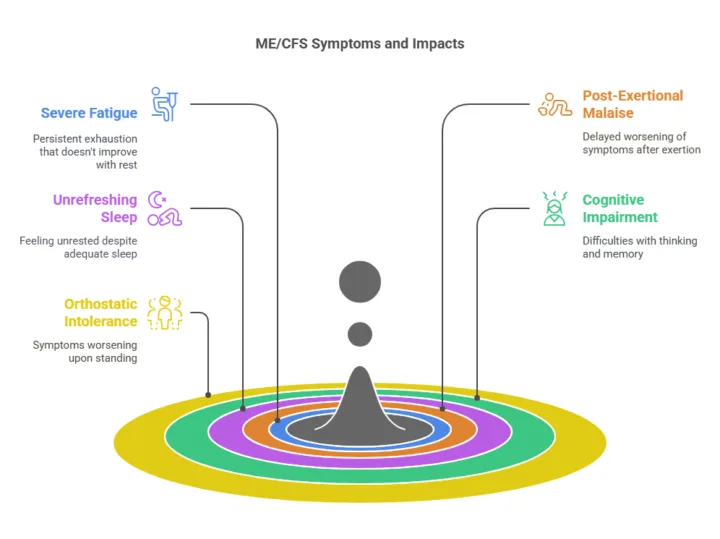
While severe fatigue is a defining feature, ME/CFS encompasses a range of disabling symptoms that can vary in intensity and presentation from person to person. The core symptoms required for diagnosis typically include:
-
Severe Fatigue: A profound and persistent feeling of exhaustion that does not improve with rest.
-
Post-Exertional Malaise (PEM): This is a critical and often delayed worsening of symptoms following even minor physical, mental, or emotional exertion. PEM can be delayed by 12 to 48 hours after the activity and can last for days or even weeks, leading to a “crash” where the individual’s ability to function is severely limited.
-
Unrefreshing Sleep: Despite spending adequate time in bed, individuals with ME/CFS often do not feel rested or restored upon waking. Sleep disturbances are common and can include difficulty falling asleep, staying asleep, or disturbed sleep architecture.
-
Cognitive Impairment (“Brain Fog”): This can manifest as difficulties with thinking, memory, concentration, information processing, and finding words. This cognitive dysfunction can significantly impact a person’s ability to work, study, and perform daily tasks.
-
Orthostatic Intolerance: Symptoms that worsen upon standing or sitting upright and improve when lying down. This can include dizziness, lightheadedness, fainting or near-fainting (syncope), rapid heart rate (tachycardia), and fluctuations in blood pressure.
In addition to these core symptoms, individuals with ME/CFS may experience a variety of other manifestations, including:
-
Muscle pain and joint pain without swelling
-
Headaches (often new or with a different pattern)
-
Sore throat
-
Tender lymph nodes
-
New sensitivities to light, sound, odors, food, or chemicals
-
Digestive issues (e.g., nausea, bloating, irritable bowel syndrome)
-
Flu-like symptoms
-
Chills and night sweats
Exploring the Triggers: A Systemic Breakdown
The exact cause of ME/CFS is not yet fully understood, but research suggests it is likely a complex interplay of factors rather than a singular issue. Potential triggers and contributing factors being investigated include:
-
Viral or Bacterial Infections: Many cases of ME/CFS are reported to begin after an acute infection, such as mononucleosis (Epstein-Barr virus), influenza, or other viral or bacterial illnesses. More recently, a significant number of individuals have developed ME/CFS-like symptoms following COVID-19 infection (often referred to as Long COVID).
-
Immune System Dysregulation: Abnormalities in immune cell function, cytokine levels, and the presence of autoantibodies (antibodies that mistakenly target the body’s own tissues) are areas of active research. It is thought that the immune system may remain in an overactive or dysfunctional state after an initial trigger.
-
Hormonal Imbalances: Dysregulation of hormonal systems, such as the hypothalamic-pituitary-adrenal (HPA) axis and thyroid function, has been observed in some individuals with ME/CFS.
-
Genetic and Environmental Factors: There may be a genetic predisposition that makes some individuals more susceptible to developing ME/CFS after exposure to certain environmental triggers.
It is important to note that ME/CFS is considered a systemic breakdown, affecting multiple bodily systems, rather than being solely attributable to one cause.
The Critical Statistic: The Undiagnosed Majority
The statistic that up to 90% of individuals with ME/CFS remain undiagnosed is alarming and highlights significant challenges within the healthcare system. Several factors contribute to this vast diagnostic gap:
-
Lack of a Definitive Diagnostic Test: Currently, there is no single blood test, imaging scan, or biomarker that can definitively diagnose ME/CFS. Diagnosis is primarily based on a thorough medical history, physical examination, and ruling out other conditions that could be causing similar symptoms. While research is actively exploring potential biomarkers, none have yet demonstrated sufficient sensitivity and specificity for routine clinical diagnosis.
-
Symptom Overlap with Other Conditions: The symptoms of ME/CFS, such as fatigue, pain, and cognitive difficulties, can overlap with many other medical conditions, leading to misdiagnosis or delayed diagnosis.
-
Lack of Awareness and Education Among Healthcare Professionals: Many healthcare providers may have limited knowledge or understanding of ME/CFS, its diagnostic criteria, and its debilitating nature. This lack of education can lead to symptoms being dismissed or attributed to psychological factors.
-
Patient Difficulty in Articulating Symptoms: The fluctuating and often unpredictable nature of ME/CFS symptoms can make it challenging for patients to clearly describe their experience to healthcare providers.
-
Stigma and Lack of Medical Validation: Unfortunately, some individuals with ME/CFS still face skepticism and a lack of validation from the medical community and society, leading to delays in seeking or receiving appropriate care.
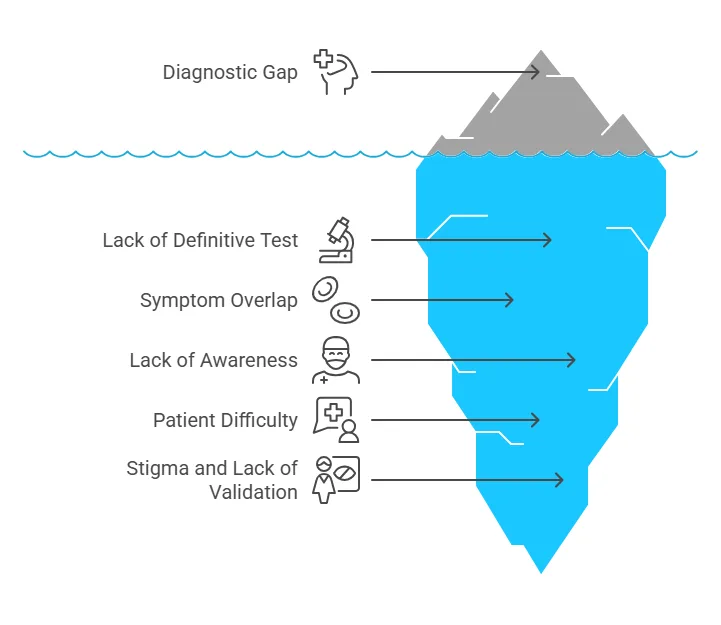 This vast gap in diagnosis means that the majority of people with ME/CFS are suffering without the medical validation, understanding, and support they desperately need.
This vast gap in diagnosis means that the majority of people with ME/CFS are suffering without the medical validation, understanding, and support they desperately need.
Who is Affected? A Health Disparity
ME/CFS can affect anyone, regardless of age, gender, or ethnicity. However, certain demographics appear to be more commonly diagnosed:
-
Gender: Women are diagnosed with ME/CFS significantly more often than men, typically at a rate of 2 to 4 times higher. This represents a significant health disparity that warrants further investigation.
-
Age: While ME/CFS can occur at any age, it is most commonly diagnosed in individuals between 40 and 60 years old. However, it also affects children and adolescents, and can occur in older adults.
-
Ethnicity and Location: Recent research highlights disparities in diagnosis based on ethnicity and geographical location, suggesting that access to knowledgeable healthcare providers and recognition of the illness may play a role.
The Cycle of Trying Harder: A Detrimental Pattern
Individuals with ME/CFS often describe a detrimental pattern known as the “cycle of trying harder.” This occurs when individuals, motivated by a desire to regain their previous level of function, push themselves beyond their physical and mental limits despite feeling unwell.
The cycle typically involves:
-
Feeling Awful: Experiencing the initial discomfort and symptoms of ME/CFS.
-
Pushing Through: Attempting to overcome symptoms and maintain activity levels through sheer willpower.
-
Triggering PEM: Exceeding their energy envelope, which triggers a delayed exacerbation of symptoms (PEM).
-
Crash: Experiencing a severe worsening of symptoms that can be profoundly disabling, often requiring extended periods of rest or bed rest to recover.
 This cycle is counterproductive and can actually worsen the long-term prognosis of ME/CFS. A key aspect of managing the illness is learning to recognize and respect the body’s limits through a strategy called “pacing.”
This cycle is counterproductive and can actually worsen the long-term prognosis of ME/CFS. A key aspect of managing the illness is learning to recognize and respect the body’s limits through a strategy called “pacing.”
Taking Action: What You Need to Know and Do
For individuals experiencing persistent, debilitating fatigue and other symptoms suggestive of ME/CFS, or for those who know someone who is, taking proactive steps is crucial:
-
Do Not Dismiss It: Do not underestimate the severity of persistent, unexplained fatigue and other associated symptoms. It is important to take these symptoms seriously and seek medical attention.
-
Seek Thorough Medical Evaluation: Consult with a healthcare professional to undergo a comprehensive medical history, physical examination, and appropriate laboratory tests to rule out other potential causes for the symptoms. Be prepared to provide a detailed account of your symptoms, their onset, duration, severity, and how they impact your daily life.
-
Advocate for Yourself: Given the challenges in diagnosing ME/CFS, it is essential to be a persistent and informed advocate for your health. Seek out clinicians who are knowledgeable about ME/CFS. If your current healthcare provider is not familiar with the illness, consider seeking a second opinion from a specialist who has experience with ME/CFS or complex chronic conditions.
Raising Awareness for Real Change
Raising awareness about ME/CFS is a critical step towards improving recognition, diagnosis, and ultimately, treatment for those affected. Understanding ME/CFS as a legitimate biological illness is fundamental to fostering accurate diagnosis and driving research efforts. Increased awareness can help reduce the stigma associated with the disease and ensure that individuals receive the medical care and support they need to manage their symptoms and improve their quality of life. Events like ME/CFS Awareness Day serve as important platforms to educate the public and healthcare community about this often-hidden illness.
In conclusion, Myalgic Encephalomyelitis/Chronic Fatigue Syndrome is a serious and complex disease with profound effects on the lives of those it touches. While challenges in diagnosis and treatment remain, increased awareness, dedicated research, and a patient-centered approach to care offer hope for better outcomes in the future. If you suspect you or someone you know may have ME/CFS, seeking a thorough medical evaluation is the essential first step towards understanding and managing this challenging condition.